Case:
A 66 year-old man presented with 2 weeks of increasing cough, generalized weakness, and decreased oral intake. He has a past medical history of a tonsillar squamous cell carcinoma for which he had received both chemo and radiation therapy. His last treatment was months prior. He was followed by the palliative care service who was managing his throat pain with hydromorphone.
He reported an increasing non-productive cough without fever, nausea, vomiting, or other systemic symptoms. He endorsed severe weakness without any focal neurologic deficit. He denied chest pain and pleuritic chest pain. He was mildly short of breath without orthopnea or paroxysmal nocturnal dyspnea.
He presented with abnormal vital signs: Temp 37.7C, HR 124, RR 18, 118/54, 84% on room air. He was a cachectic man with dry mucous membranes. There was no increased work of breathing. Neurologic, Cardiac, resp, and abdominal exams were normal. There was no unilateral calf swelling or tenderness.
POCUS Findings
Pericardial effusion was excluded.
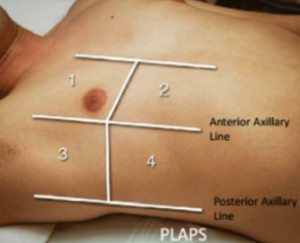
Thoracic ultrasound revealed normal lung sliding bilaterally. We divide our thoracic ultrasound regions according to these boundaries:
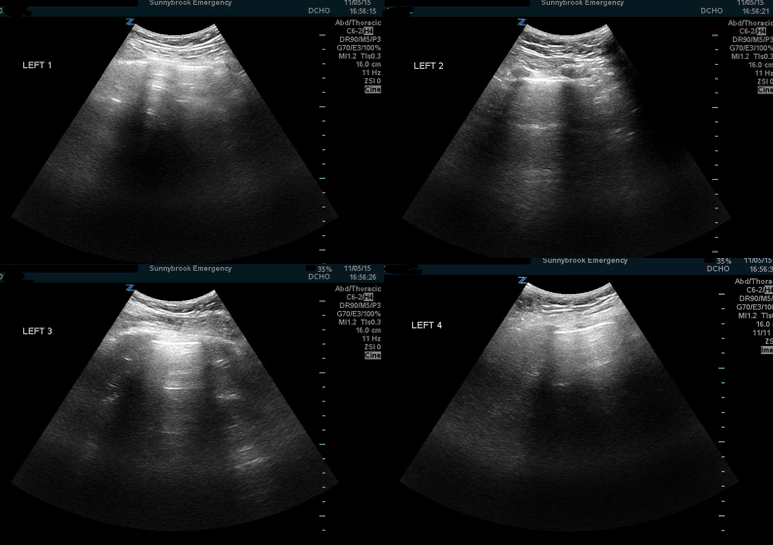
Left hemithorax demonstrated normal A-line patterns with no evidence of B-lines or effusion:
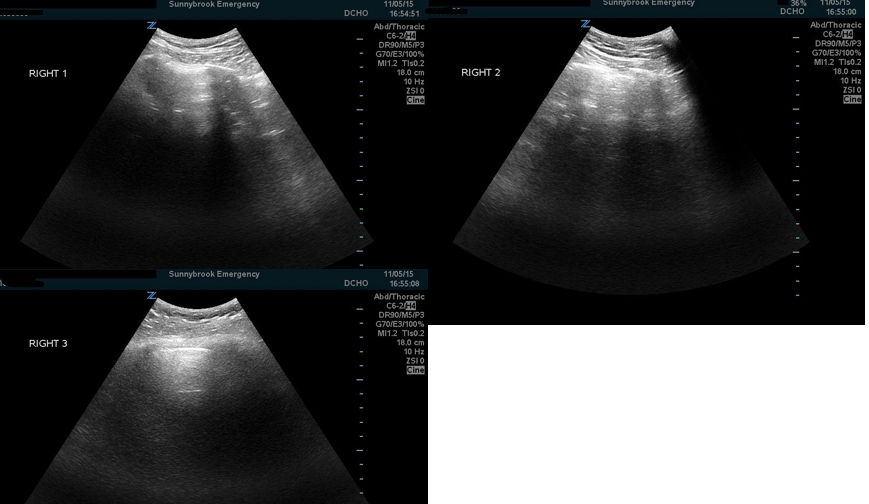
Right hemithorax:
The R4 and R PLAPS region demonstrated evidence of a focal B-line pattern. Note how multiple B lines can coalesce creating a “gigantic B line” also called a “lung rocket”. Also note how the B lines exist in multiple intercostal spaces.
There was a focal B line pattern in the R4 and PLAPS region. There were greater than 3 B-lines in each costal region over two intercostal spaces demonstrating a positive scan and evidence of alveolar interstitial syndrome (see below).
Differential and Management:
Full septic work up and treatment with IV fluids was initiated. CXR was normal.
Based on ultrasound findings of this focal AIS pattern, cough, SIRS criteria, hypoxemia, empiric therapy for CAP was initiated with ceftriaxone and azithromycin.
A CT scan was obtained to rule out pulmonary embolism.
CT demonstrated:
CT scan demonstrated bilateral pulmonary emboli to an interlobal, segmental, and subsegmental level. Right ground-glass opacities consistent with right upper lobe pulmonary hemorrhage.
Case Resolution:
Our patient had bilateral pulmonary embolisms and resultant pulmonary hemorrhage. He was treated empirically for CAP and was admitted to medical oncology whereafter he was anticoagulated and currently remains in hospital.
Differential for Alveolar Interstitial Syndrome (AIS):
Positive region: 3 or more simultaneous B lines in a single intercostal view
Positive scan = alveolar interstitial syndrome: 2 or more positive regions in one hemithorax
AIS is a syndrome and like most syndromes, there is a differential:
Pulmonary Hemorrhage Added to the Differential of Focal AIS!
The focal AIS that we detected in the right hemithorax in the R4 and PLAPS region was actually a pulmonary hemorrhage! Here’s a great reminder that AIS has a differential that should be considered. We initially made a cognitive error of premature closure – AIS+s/s of pneumonia = pneumonia. But not necessarily. We suggest that pulmonary hemorrhage should be on the differential for focal AIS. A quick search of the literature reveals no reported cases of pulmonary hemorrhage detected on point-of-care ultrasound.
Learning Points:
- Be methodical about scanning the lung and scan multiple regions using the convention we suggest above. It would be really easy to miss focal areas of AIS if you only scan a single region.
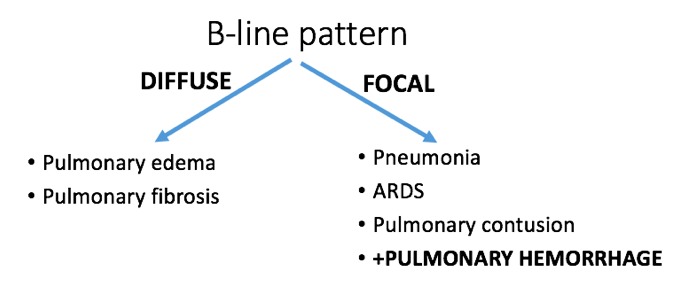
- The differential for alveolar interstitial syndrome is broad, but can be narrowed based on the distribution of B-lines.
- Focal B-lines are the most non-specific findings of a consolidation (hepatization, dynamic air bronchograms, and the shred sign are more specific).
- Consider adding pulmonary hemorrhage to the differential for a focal B-line pattern.
- The Meaning of B-Lines - November 15, 2015
- Does shoulder dislocation = 2 x-rays? - August 16, 2015